 Managing accounts receivable in medical billing and handling claim denials is one of healthcare providers’ most significant challenges in revenue cycle management (RCM). Unpaid claims, delayed reimbursements, and high denial rates can significantly impact cash flow, leading to financial instability.
Managing accounts receivable in medical billing and handling claim denials is one of healthcare providers’ most significant challenges in revenue cycle management (RCM). Unpaid claims, delayed reimbursements, and high denial rates can significantly impact cash flow, leading to financial instability.
Healthcare providers must adopt proactive accounts receivable and denial management techniques to maintain a steady cash flow and reduce write-offs. By implementing robust strategies, medical billing teams can prevent denials, streamline collections, and optimize revenue cycles.
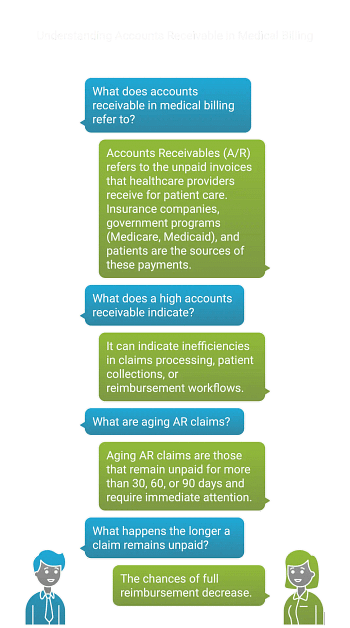
Accounts receivable in medical billing refers to the outstanding payments due to a healthcare provider from insurance payers and patients for medical services rendered. A high AR can indicate inefficiencies in claims processing, patient collections, or reimbursement workflows.
Aging AR claims that remain unpaid for more than 30, 60, or 90 days are red flags that require immediate attention. The longer a claim remains unpaid, the lower its chances of full reimbursement.
One of the most effective ways to reduce outstanding accounts receivable in medical billing is to prioritize them based on age, value, and collectability. Older accounts are more likely to become uncollectible, making them a top priority for collection efforts. Additionally, larger accounts should be given precedence, as they significantly impact the organization’s financial health.
Focusing on accounts with verified insurance coverage and minimal disputes can also improve collection efficiency. Healthcare providers can maximize recovery rates and minimize financial losses by implementing a structured prioritization system.
Billing errors are a significant cause of claim denials and payment delays. Verifying patient details, insurance information, and billing codes before submitting claims is critical to reducing AR. Providers should:
By ensuring accurate billing information upfront, providers can prevent denials and accelerate reimbursements, leading to a healthier revenue recovery.
Consistent follow-ups with patients and insurance companies help maintain AR efficiency. Setting up automated reminders, phone calls, and emails ensures that outstanding balances remain top-of-mind for payers. Regular follow-ups can:
By establishing a structured follow-up system, healthcare providers can minimize unpaid bills and enhance financial stability.
Not all patients can pay their medical bills in full immediately. Offering structured payment plans makes it easier for patients to clear outstanding balances while improving collection rates. Consider these strategies:
Flexible payment solutions improve cash flow while maintaining positive patient relationships, leading to long-term financial success.
Despite best efforts, some accounts may become uncollectible. Writing off bad debt is sometimes necessary, but it should be done strategically. Before writing off an account, providers should:
By effectively managing uncollectible accounts, providers can maintain accurate financial records, reduce audit risks, and keep revenue cycle operations efficient.
Regulatory compliance is crucial in preventing claim denials and financial penalties. Healthcare providers must stay informed about the latest billing and collections regulations, including Medicare, Medicaid, and private insurance policies. To ensure compliance:
A proactive approach to regulatory compliance minimizes financial risks and improves AR performance.
Well-trained staff play a vital role in effective AR and denial management. Employees handling billing and collections should be well-versed in:
Ongoing training ensures staff members stay updated on industry trends and regulations, leading to a more efficient revenue cycle.
Effective denial management is key to recovering lost revenue. A structured approach ensures denied claims are corrected and resubmitted promptly.
Ensuring accurate patient demographics, insurance eligibility, and benefits verification before services are rendered is crucial. This step helps prevent claims rejections due to incorrect or missing information. Registration errors and eligibility issues account for nearly 27% of denials, making proactive verification an essential practice.
Complete and precise patient documentation ensures payers receive a clear depiction of the patient’s condition and treatment. Accurate medical coding helps providers secure optimal reimbursement and reduces the risk of claim denials. Government programs and insurance companies rely on precise coding to determine payment, making thorough documentation a necessity.
By systematically tracking and analyzing denial trends, healthcare providers can identify recurring patterns, such as common denied services, specific codes, or payer-related issues. This data-driven approach allows organizations to implement corrective actions, such as updating documentation practices, refining coding guidelines, or negotiating better terms with payers. Continuous monitoring of denial trends also ensures revenue cycle improvements over time.
A lack of knowledge about denial management often leads to increased claim rejections. Providing staff with ongoing education on documentation accuracy, coding compliance, and claims submission guidelines enhances their ability to prevent denials. Hiring an experienced revenue cycle management partner can further streamline the process, improve compliance, and identify revenue enhancement opportunities.
Creating a specialized denial management team allows organizations to focus on identifying and resolving the root causes of claim denials. This team should include members from coding, billing, and clinical departments to enhance collaboration and reduce information gaps. A dedicated team fosters accountability and ensures that denial prevention strategies are effectively implemented and continuously improved.
Routine audits help uncover errors in coding, documentation, and billing practices before they result in claim denials. Audits also ensure compliance with regulations, reducing the risk of penalties and fines. By identifying inefficiencies such as outdated technology or manual processes – healthcare providers can enhance operational efficiency and reduce revenue leakage.
Tracking KPIs allows providers to assess the effectiveness of their denial management strategies. Monitoring metrics such as denial rates, appeal success rates, and reimbursement timelines help organizations set realistic goals and allocate resources efficiently. Understanding the financial impact of denials enables data-driven decision-making and continuous improvement in revenue cycle performance.
To measure the effectiveness of AR and denial management strategies, healthcare organizations should monitor these key performance indicators (KPIs):
FAQs
Accounts receivable (AR) refers to outstanding payments owed to healthcare providers by insurance companies or patients for medical services rendered.
Providers can reduce AR by verifying patient information, prioritizing collections, implementing follow-ups, offering flexible payment plans, and ensuring accurate billing.
Claim denials often occur due to incorrect patient information, coding errors, lack of documentation, expired insurance, or non-covered services.
Effective denial management includes tracking denial trends, ensuring accurate coding, educating staff, and resubmitting corrected claims promptly.
Important KPIs include Days in AR (<30 days), Denial Rate (<5%), First Pass Resolution Rate (>90%), and Appeal Success Rate (>70%).
Managing claim denials and accounts receivable in medical billing is essential for maintaining a healthy revenue cycle. By taking proactive steps such as automating workflows, improving patient collections, and refining denial management strategies, healthcare providers can enhance cash flow and reduce financial risks.
If your practice is struggling with high AR or frequent claim denials, EZ Settle Solution offers expert medical billing and coding services to optimize your revenue cycle.