Even though mental health treatments are critical to the overall health of patients, it remains a significant challenge for healthcare providers to fulfill their billing and reimbursement obligations in an appropriate manner. The billing process for mental health services is challenging due to the presence of complicated coding requirements, frequent policy changes, and intricate coding guidelines. It is possible for healthcare providers in the United States and the United Kingdom to maximize revenue, reduce the number of claims that are denied, and speed up the process by outsourcing professional medical billing firms such as EZ Settle Solutions.
In this blog, we will examine the complexities of mental health medical billing, essential compliance considerations, and ways to secure timely reimbursements. But before that, let’s understand behavioral health billing.
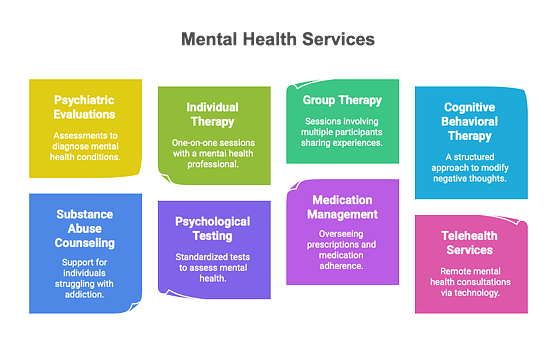
Mental health billing is also known as behavioral health billing. It is the practice of recording and submitting mental health insurance claims for payment of services provided by mental health professionals. Therapy sessions, mental health assessments, medication management, and more are all included in the extensive range of services. Billing for mental health treatments frequently entails dealing with government programs such as Medicare and Medicaid, private insurance companies, and direct payments from individuals who pay for their own care.
Compliance with mental health medical billing rules, regulations, and ethics applies to the entire billing process. Non-compliance can result in financial penalties, legal issues, damage to professional reputation, and harm to patients.
Here are the reasons why behavioral health billing compliance is crucial.
Billing procedures by mental health professionals must be transparent and ethical. Truthful billing builds confidence between physicians and patients and promotes beneficence and non-maleficence.
Billing violations can result in fines, civil penalties, and criminal charges for fraud or abuse. Mental health professionals must follow HIPAA compliance, the False Claims Act, and state billing standards.
The financial sustainability of mental health practices depends on billing compliance. With timely and accurate compensation, practitioners can continue to deliver exceptional care without financial burden. Compliance with insurance company regulations reduces claim denials and payment delays.
Insurance firms, government organizations, and regulatory authorities audit mental health practices for billing compliance. Maintaining precise paperwork and following billing standards can reduce audit results and penalties.
Insurance regulations and coverage guidelines for mental health services are continuously changing, so providers must stay up to date to avoid claim denials.
The complexity of diagnostic coding systems, including the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT), presents challenges for precise billing. Mental health diagnoses frequently include multiple disorders and complex signs and symptoms, requiring careful selection of suitable codes.
Accurate documentation is required for correct coding and reimbursement. Missing or improper documentation may result in claim denials.
Mental health services frequently receive lower reimbursement rates than other medical specialties, making it critical to maximize claim accuracy.
Many insurers need prior authorization for mental health treatments, which can delay service delivery if not handled appropriately.
A high incidence of claim denials for mental health care can reduce income. Knowing how to appeal refused claims is critical to financial stability.
Even with the problems, mental health professionals can follow a few best practices to help mental health facilities get their bills paid on time:
Administrative staff must be fully trained on billing processes, coding guidelines, and regulatory requirements to stay compliant. This training helps keep staff proficient in billing procedures.
Using EHR systems with built-in billing tools makes the processes of documenting, coding, and sending in mental health insurance claims easier. EHR systems also have built-in checks to make sure they follow payment rules. This lowers the chance of mistakes and missed tasks.
Internal audits of billing methods conducted regularly can help find potential compliance issues and ways to improve. Practices can take action to address compliance issues by carefully checking documentation, coding, and claims handling.
Talking to professional billing services or getting advice from billing experts such as EZ Settle Solutions can help you understand complicated billing problems and government rules. Working together with pros can help practices handle billing problems better.
Encouraging a culture of compliance within the practice makes staff members more aware of how important it is to use fair billing practices. Promoting open communication, accountability, and following set rules creates an atmosphere where billing compliance is a top priority.
EZ Settle Solutions streamlines your revenue cycle with customized medical billing and coding.
Our mental health medical billing knowledge guarantees the following:
Compliance makes sure that billing is done in a legal and moral way, keeps you from getting fined, and cuts down on claim rejections so that reimbursements go smoothly.
Problems that often arise are too frequent policy changes, complicated coding, low reimbursement rates, the need for prior authorization, and high claim rejection rates.
Train your staff, use electronic health record (EHR) systems, do regular checks, work with billing experts, and encourage everyone to follow the rules.
EZ Settle Solutions ensures that claims are sent in correctly, reduces rejections, speeds up reimbursements, and follows all billing rules.
Mental health medical billing is complicated and requires strategic planning. By following best practices, rules, and professional billing services, healthcare practitioners can maximize reimbursements and focus on patient care.
Do you have mental health medical billing issues?
Call EZ Settle Solutions at 346-335-4093 / info@ezsettlesolutions.com today to optimize your billing process and maximize refunds.
Let us manage the complications so you may provide excellent mental health treatment.