One of the fastest-growing practices in healthcare is orthopedics. According to the American Academy of Orthopaedic Surgeons, approximately 12% of orthopedic practitioners operate private practices, while the rest are part of more extensive healthcare networks or consolidated with other specialties.
Whether you are running a private orthopedic practice or part of a collective practitioner, managing the financial side of your business is just as crucial as patient care. While some practitioners handle billing in-house, others rely on specialty medical billing, such as agencies like EZ Settle Solutions. Regardless of your approach, understanding the complexities of the revenue cycle in orthopedics billing is essential.
This article is specially crafted to help you understand the complexity of orthopedic medical billing, its challenges, and its solutions.
Let’s start!
Orthopedic medical billing is the process of submitting claims for services related to musculoskeletal treatments, including surgeries, physical therapy, and durable medical equipment (DME). Any inaccuracies in billing can lead to claim rejections or compliance issues, given the specificity required in coding and documentation.
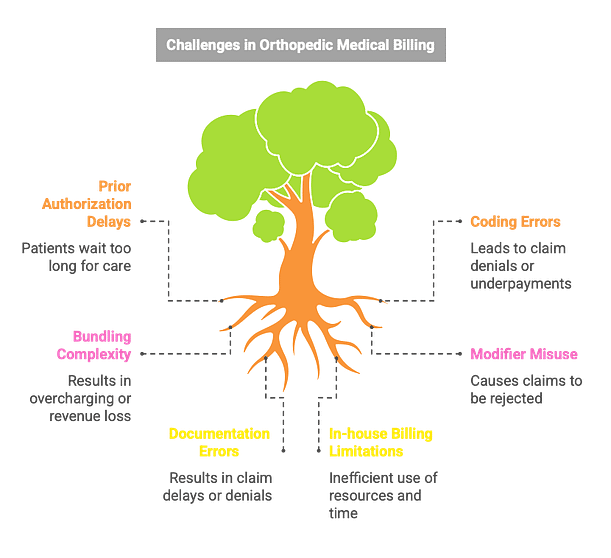
According to an American Medical Association survey, obtaining prior authorizations typically takes 16 hours per week for each healthcare provider. This figure is believed to be as high as 30 for orthopedic practices. If the medical billing and coding agencies don’t properly manage prior authorizations, your patients could have to wait one to five days before receiving the proper care. When they frequently have to wait a long time for prior authorizations, many patients quit the clinic.
Healthcare has coding problems in every field, and orthopedics is no different. Orthopedic procedures involve multiple CPT codes for orthopedics. Additionally,
there are always new versions of ICD codes, and right now, ICD-10 is used in the US. On the other hand, medical billing and coding agencies and practitioners in the US will soon use the ICD-11 version. That means coders need to learn new ways to code. If your billing and coding team hasn’t already started this process, you will be behind schedule. However, Incorrect coding or missing modifiers can lead to claim denials or underpayments.
Bundling is the practice of grouping numerous related procedures under a single payment, which is common for orthopedic services. This makes orthopedic medical billing and coding more difficult due to the complexity of understanding bundled code. Orthopedic practitioners have to be aware of which processes are bundled with them to prevent overcharging or undercharging, which may result in claim denials or revenue loss.
For example, if the scheduled series injection was carried out on the same day, the EM services are not individually billable. If the EM service is not a planned/follow-up for an infusion, it can be billed with a modifier 25/24/57 and a distinct diagnosis associated with EM, as opposed to injections or any other bundled services.
When paying for orthopedic care, it’s very important to use modifiers correctly, especially when treatments are done on more than one part of the body. Claims are often turned down because the factors are wrong or missing. Modifiers are also useful for correctly explaining operations like revisions and surgeries on both sides. It can be hard to figure out NCCI (National Correct Coding Initiative) changes, which say when modifiers like Modifier 59 can be used to avoid certain code pair edits.
Insufficient or incorrect documentation is one of the leading causes of claim rejections in orthopedic billing. Missing details such as medical necessity, procedure descriptions, or supporting clinical notes can result in delays or outright denials from insurance payers. Providers may also fail to update patient records properly, leading to inconsistencies in claims submissions.
Nowadays, having an internal medical billing and coding team is quite acceptable for an orthopedic clinic. While the other team handles coding and invoicing, staff members can focus just on practice and patient.
However, outsourcing medical billing and coding companies may be a better option in the following cases.
Electronic health record (EHR) systems and automated tools establish a productive prior authorization workflow. Committed billing teams should monitor payer requirements and make requests as soon as possible to prevent treatment delays. Collaborating with a skilled medical billing business can reduce administrative costs and streamline the process.
Providing regular training and instruction on ICD-10 and CPT Coding upgrades can improve coding accuracy. Hiring professional coders with expertise in orthopedic billing can avoid coding problems. Coding software and AI-powered billing systems can also improve accuracy and adherence to changing rules.
Orthopedic clinics should be thoroughly aware of bundled codes to guarantee correct billing. Billing teams should apply the proper modifiers when needed and periodically review the National Correct Coding Initiative (NCCI) rules. Routine audits can reduce claim denials and identify improper bundling.
To prevent rejected claims, teaching programmers how to properly use modifiers is essential. Practices should evaluate payer rules on modifier needs and keep an updated modifier reference guide. Before submission, automated claim-scrubbing systems can identify missing or inaccurate modifiers.
Use standardized documentation templates to record all necessary data before submitting a claim. Billing teams should perform routine audits to find and fix discrepancies, and physicians should be trained on appropriate documentation procedures. EHR systems with integrated compliance checks can reduce errors.
Orthopedic clinics should assess their billing volume and decide whether outsourcing is a more cost-effective solution. If in-house billing is preferred, investing in sophisticated billing software and training can increase productivity. Outsourcing to specialized medical billing firms can raise reimbursement rates and decrease administrative expenses.
There are many challenges with orthopedic medical billing, including complicated coding, documentation errors, and delays in prior authorization. However, with the correct tactics, such as appropriate training, the use of cutting-edge billing software, and, when needed, outsourced medical organizations like EZ Settle Solutions, practices may optimize their revenue cycle and guarantee precise, on-time reimbursements. Orthopedic clinics can maximize their cash flow and concentrate on providing high-quality patient treatment by proactively tackling these typical issues.
For more assistance, connect with us at 346-335-4093 / info@ezsettlesolutions.com or schedule a free consultation to learn more about how we can assist you.