Are your practices facing an Emergency Room Medical Billing issue?
If yes, then this blog is for you.
Hospitals include various facilities such as orthopedics, gastroenterology, cardiology, rheumatology, etc., and the emergency room is one of them. This service operates 24/7 and ensures that each patient receives immediate care at any time. This means the emergency room handles various medical emergencies, from minor injuries to acute illnesses, making it a critical component of hospital services.
Despite this, emergency room billing is a complex process. Unlike the other department, where patients often visit with appointments, this department has to deal with patients who need emergency care, which further complicates the emergency room medical billing process.
However, Successful emergency room medical billing requires a well-coordinated approach that involves precise coding, accurate documentation, knowledge of compliance rules, and clear communication between healthcare professionals and billing teams.
Now let’s understand this in depth!
In this blog, we will discuss emergency room medical billing, its importance, and strategies to increase the precision, effectiveness, and profitability of emergency department billing.
Let’s start!
Emergency room medical billing is the process of submitting a claim for services that a patient receives in the emergency department. The billing process for this department is quite complicated due to the urgent services, the involvement of several healthcare providers, and the various insurance policies that control emergency department reimbursement. Additionally, the hospital charges fees for various ER resources such as medical assets, supplies, and administrative costs. These fees vary based on the hospital and the complexity of care provided.
ER billing includes various challenges that require proper management to reduce claim denial and ensure appropriate emergency department reimbursement. Here are a few key challenges. Let’s have a look:
Since the ER operates 24/7, physicians have to deal with a high volume of patients with multiple health issues or diagnoses. Additionally, most patient visits are unplanned, and many are admitted without proper documentation, leaving no time for physicians to explain the insurance process to patients.
As a result, claims have been submitted with incomplete or incorrect information, resulting in delays or denials.
One of the most common challenges physicians face is complex coding and documentation.
As a specialized medical unit, the ER has to handle multiple patients with various medical conditions, from minor injuries to life-threatening emergencies. And each case may require specific ICD-10 and CPT codes per the ER coding guidelines, which complicates the coding and documentation process.
In emergency conditions, patients often visit without insurance documentation or complete insurance coverage information, making verification and the eligibility process difficult. Additionally, failure to obtain prior authorization may result in claim denial or delay in reimbursement.
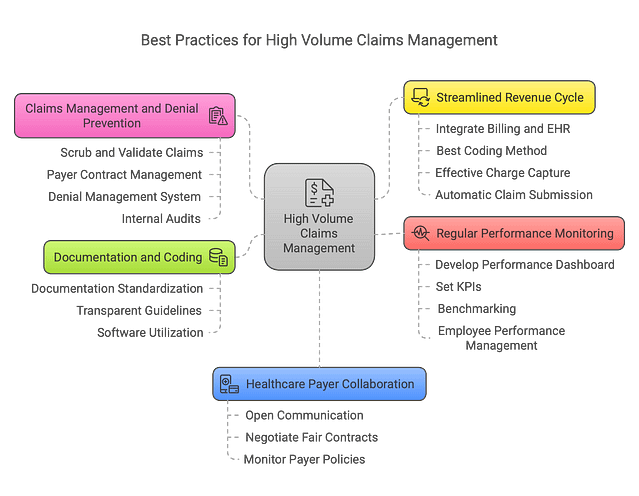
Correct documentation and coding are key to healthcare billing. This improves patient treatment and the faster reimbursement process. Here are the methods to improve documentation and coding accuracy:
Use an easy-to-fill-out documentation template. It should also list all the relevant patient’s health information. Additionally, it encourages healthcare providers to supply information needed for accurate billing and coding. This process will help manage the capture of high-volume patients’ data.
Create transparent coding accuracy documentation guidelines. Guidelines must reflect daily ER billing industry changes. This reduces errors in coding and documentation, resulting in accurate claim submission with zero denials.
Use software to analyse all documents and suggest improvements. This reduces the chances of error in documentation and coding.
A good healthcare revenue cycle requires effective claims and denial prevention. Avoiding refused claims and managing them can improve cash flows and reduce administrative costs. Ways to improve claims handling and avoid denials:
Automates scrubbing process for high-volume patient claim submissions. Before submitting claims, this software checks for all errors. Validate before submission. Verify all papers and coding accuracy.
Addressing any difficulties with healthcare insurance companies requires clear communication. Healthcare professionals should learn payer contract basics. This assures exact insurance claim processing.
Due to frequent denial, emergency room medical billing becomes complicated. Use a denial management system to handle denials efficiently. Automated software tracks and responds to allegations.
Regular internal audits discover claims concerns before submission. Audit results help healthcare professionals identify and prevent denials.
Administrative practices optimizing the healthcare revenue cycle are essential for accurate payments, lower administrative costs, and timely financial performance. Here is how to simplify the revenue cycle:
EHR and billing integration is essential for emergency room RCM. Data input by hand causes many errors. EHRs reduce denials and rejections. It improves accuracy and speeds charge capture.
Hire ICD-10 and CPT-savvy coders. Assign codes properly. Coders can also use tools to organise their coding.
Use barcode scanners and mobile apps. This technique collects charges well. Regular internal audits help the supplier gather charges appropriately without faults or concerns.
The automation of claim submission via EDI has been proven. This boosts the company’s clean claim ratio. Clearing houses verify claims.
Partnership with the payer is an essential step in healthcare revenue cycle management. This step streamlines the high-volume patient claim submission process and hastens the reimbursement.
Here is how to do it:
Open and regular communication between the healthcare provider and insurance company fosters collaboration. Issues are resolved immediately.
The contract between the two parties should be unambiguous to avoid confusion. Clear conditions and reimbursement rates ensure fair collaboration and contract compliance.
Keep up with healthcare payer policy changes and learn from payer portals. This keeps the healthcare organisation compliant and decreases claim denials.
Monitoring performance routinely helps healthcare organisations maintain efficiency, identify areas for improvement, and ensure proper functionality. Effective frequent performance monitoring includes these features and strategies:
Performance dashboards assist insurance companies and patients in evaluating healthcare organisations. These dashboards show live metrics.
Healthcare revenue cycle KPIs measure emergency room effectiveness. Key KPIs include Clean claims, Bad Debt rates, and Charge Lag.
Benchmarking compares an organization’s performance to industry competitors. This identifies areas for improvement.
Install regular monitoring. Employee performance is easily assessed. Develop employee professional development goals and opportunities.
The urgency, high patient volume, and absence of prior documentation or insurance verification complicate emergency room charging. ER services demand precise coding and payer policy compliance from numerous healthcare providers.
Most denials are due to insufficient or erroneous documentation, coding problems, absence of prior authorisation, and insurance verification issues.
Correct and complete documentation, automated claim scrubbing technologies, regular audits before submission, and open contact with insurance carriers help reduce denials for hospitals.
Billing automation reduces errors, improves claim accuracy, and speeds reimbursement. EHR integration, automatic cleansing, and denial management boost efficiency.
Open communication, creating explicit contracts, remaining current on policy changes, and reviewing performance metrics improve payer collaboration and claim processing.
Efficient emergency room medical billing is essential to guarantee seamless financial operations in healthcare facilities. Healthcare providers must use strategic billing methods given the many claims, complicated coding rules, and insurance verification difficulties. Hospitals can maximise their revenue cycle using standardised documentation and automation, keeping open contact lines with payers and regularly tracking performance. A proactive strategy reduces claim denials and speeds payment, improving financial stability and patient care.